You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
With the passing of the Occupational Safety and Health (OSH) Act in 1970, the US Congress created the Occupational Safety and Health Administration (OSHA). The agency was designed to ensure the safety and health of working men and women by setting and enforcing standards and by providing training, outreach, education, and assistance.1
The OSH Act of 1970 assigns responsibility for worker safety to employers. This is accomplished through standards (ie, regulations) issued by OSHA. When no standard exists for a safety-related situation, OSHA’s General Duty Clause applies as a blanket regulation.2 The General Duty Clause states that each employer has two responsibilities: (1) to furnish each employee a place of employment free from recognized hazards that are causing or are likely to cause death or serious physical harm to employees; and (2) to comply with promulgated occupational safety and health standards. Each employee must comply with occupational safety and health standards and all rules, regulations, and orders that are applicable to their own actions and conduct.3
This means both employers and employees have rights and responsibilities. Both parties must work cooperatively to establish and maintain a safe and healthy working environment. There can be no rights without commensurate responsibilities.
Currently, there are no OSHA standards specific to dentistry. However, dental workers are exposed to numerous biological, chemical, environmental, physical, and psychological workplace hazards. Standards are available that help protect the safety and health of all healthcare workers, including those in dental workplaces. Examples include the standards for bloodborne pathogens, hazard communications, and ionizing radiation.4-6
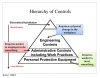
Hierarchy of Controls
A variety of prevention and control mechanisms are designed to protect workers from workplace hazards. Employers should select the controls that are the most feasible, effective, and permanent for their workplace. A hazard control plan describes how the selected controls will be implemented. An effective plan addresses serious hazards first. Interim controls may be necessary, but the overall goal is to ensure the presence of successful long-term control of hazards. Controls that could potentially directly or indirectly introduce new hazards should be avoided. Examples include exhausting contaminated air into occupied workspaces or using hearing protection that makes it difficult to hear conversations or alarms.7
OSHA has prepared a diagram that visually explains a hierarchy of interrelated controls (Figure 1).8
The most effective control is elimination (ie, physically removing a hazard) and substitution (ie, replacing the hazard). For example, it may be possible to move a hazardous process to another location. Or perhaps the work could be sent to an outside vendor. Also, glutaraldehyde solutions should not be used for environmental disinfection. Rather, EPA-registered hospital disinfectants with tuberculocidal claims (eg, chlorine-based products, phenolics, and iodophors) should be used, which are effective and safer to workers and environmental surfaces.7,8
Engineering controls are designed to isolate workers from a hazard. They require a physical change in the workplace. Examples include devices (eg, sharps disposal containers and self-sheathing needles) that isolate or remove bloodborne pathogen hazards from the workplace.7,8
Administrative controls include work practice controls that change how work is performed, ie, workers and employers find an alternative process. Such controls reduce the likelihood of exposure by modifying the manner in which a task is performed (eg, prohibiting recapping of needles by a two-handed technique).7,8
Personal protective equipment (PPE) (eg, gloves, masks, protective eyewear, gowns) is the least protective type of control. PPE controls require workers to wear something. PPE is specialized clothing or equipment worn by an employee for protection against a hazard. General work clothes such as uniforms, pants, shirts, or blouses not intended to function as protection against a hazard are not considered to be PPE.7,8
Different types of PPE can be used alone or in combination to provide the desired level of protection. PPE selection is based on the task(s) being performed and the anticipated level/type of exposure hazard expected. It is important to track progress toward completing the hazard control plan and periodically (at least annually and when conditions, processes, or equipment change) verify that controls remain effective.7
Using PPE
If PPE is to be used as a control, then the facility should implement a PPE program. This should address the hazards present; the selection, maintenance, and use of PPE; and the training of employees. Again, PPE is the least effective control mechanism for protecting workers from hazards. All PPE has protective value but also inherent limitations.
An increase in the use of PPE in the dental setting began in the early 1980s with the emergence of HIV/AIDS. PPE use has been a long-debated topic. Product selection and usage is important, but problems can occur that must be considered. There are three criteria that can help the selection process; they involve three terms: reasonable, necessary, and appropriate. Is the PPE in question a reasonable request? For example, protective eyewear is a reasonable request for dental workers, while a self-contained breathing apparatus may be reasonable in some orthopedic surgery situations but not in dental offices. The term necessary means required or needed. Gloves are necessary in a clinical setting and supported by scientific evidence.9 Appropriate indicates that there are choices. Some PPE is more protective in certain situations than other types, and selection should be based on the kind of exposure expected. For example, heavy-duty, heat-resistant gloves are appropriate when removing sterilized instruments from an autoclave, while clinical gloves would be inappropriate.
Other factors also influence selection and use of PPE. The nature of a hazard dictates the amount and types of PPE needed. The culture or tradition in the office plays a role, as workers are inclined to do things the way they’ve been done in the past. Proper fit and visual appeal also affect workers’ choices to use PPE; comfort will typically improve compliance. PPE must also be biocompatible (hypoallergenic). The use of latex has been diminishing. PPE should also have longevity, including shelf-life. Having workers be part of the selection process also is helpful.
For dental environments, there are four general types of PPE: masks, gloves, eye/face protection, and protective clothing (gowns).
Masks (Surgical/Procedural)
The use of masks in healthcare started in the early 20th century to limit practitioner microorganisms from contaminating sterile materials or surgical wounds. Masks were considered a form of respiration protection. Today, masks are known to protect both patients and practitioners.
Efficient, properly fitting masks can collect spatter, spray, and some aerosols. Infectious agents are caught on/in the mask’s surface and inner layers. Most masks in dentistry can to some degree reduce the chances of inhaling aerosolized oral fluid particles.10
Masks are made of multiple layers (generally three) of varying synthetic materials. The composite should filter a minimum of 95% of small particles, including bacteria.11 Some masks have higher filtration rates. The particles become trapped. However, masks can become overloaded if worn for extended periods (eg, 20 to 30 minutes), especially if the contamination challenge is heavy. Masks can become moist (fluids coming in and out), decreasing filtration markedly.
Dental healthcare personnel should wear a surgical mask that covers both their nose and mouth during procedures and patient-care activities that are likely to generate splashes or sprays of blood or body fluids. A surgical mask protects the patient against microorganisms generated by the wearer and protects dental healthcare personnel from large-particle droplet spatter that may contain bloodborne pathogens or other infectious microorganisms. When a surgical mask is used, it should be changed between patients or during patient treatment if it becomes wet. Masks should be paired with appropriate work practices such as the use of dental dams, and high-velocity evacuation should minimize droplets, spatter, and aerosols.10,12
Masks should be worn chairside when spraying or spattering of fluids is expected. It is also important to wear masks during instrument processing, when there is a chance of splashes and aerosols during ultrasonic cleaning and instrument rinsing.
Available in a variety of shapes, sizes, and colors, there are two basic types of masks: domed and rigid; and pleated or folded pliable. They can be secured with ear loops, ties, or headbands. An ideal mask has both high breathability and fluid resistance. Unfortunately, these are opposing characteristics. Therefore, there should be a balance of these two characteristics, and excessive moisture on the mask should be avoided. Finally, masks typically do not fit perfectly around the edges, allowing unfiltered air in and out. The optimum masks are those that fit best.10,12
Gloves
Dental personnel wear gloves to prevent hand contamination when touching mucous membranes, blood, saliva, or other potentially infectious materials (direct contact with non-intact skin) and to reduce the likelihood that microorganisms on their ungloved hands will be transmitted to patients during dental patient-care procedures (indirect contact). Like masks, gloves protect both patients and practitioners.10,12
The type of glove used is based on the type of procedure to be performed (eg, surgical versus nonsurgical or housekeeping procedures). Medical-grade nonsterile examination gloves and sterile surgical gloves are medical devices regulated by the US Food and Drug Administration (FDA). General-purpose utility gloves are not regulated because they are not promoted specifically for medical use. Sterile surgical gloves must meet standards for sterility assurance established by the FDA and are less likely than nonsterile examination gloves to harbor pathogens that may contaminate a wound.10,12
The Centers for Disease Control and Prevention (CDC) has prepared a table describing characteristics of common glove types (Table 1).12
Dental personnel should wear some type of disposable glove for patient-care activities where there is a possibility for direct hand contact with patient body fluids and/or teeth. Such gloves should also be worn when touching/handling contaminated items and surfaces.10
Gloves are single-use, disposable devices. They should never be used on subsequent patients. Washing of latex gloves, either with plain soap, a disinfectant, or alcohol, can result in micro punctures. This can lead to wicking, which may allow liquids to penetrate through undetected holes in the glove. Therefore, washing of gloves is not recommended.12
Sterile latex or vinyl gloves are used for surgical procedures. These are higher-quality gloves that come in half-sizes and dedicated left and right handed, affording superior fit.
On December 16, 2016, the FDA issued a final rule banning powdered medical gloves beginning on January 19, 2017. The ban involves most powdered medical gloves and applies to patient examination gloves, powdered surgeon’s gloves, and absorbable powder for lubricating gloves. Various types of powder have been used to lubricate gloves so that wearers could don them more easily. However, the use of powder on medical gloves presents numerous risks to patients and healthcare workers, such as inflammation, granulomas, and respiratory allergic reactions.13,14
Patient-care gloves afford considerable protection against body fluids and chemicals (direct contact). However, they offer little prevention against sharp objects such as needles, broken glass, and instruments. Mini-pores, rips, and tears also may allow passage of patient body fluids and chemicals. Utility gloves have more puncture resistance, but over time can crack and peel. No glove with defects should ever be used.10
Practitioners and patients may experience adverse reactions when contacting latex gloves. Natural and modified latex proteins and chemicals used in manufacturing are problematic. There have been attempts to reduce the amount of latex proteins present by rinsing. Repeated latex exposure can increase the chances for the development of allergies. Latex is also found in numerous other items used in dentistry, such as rubber dams, bite blocks, mixing bowls, and anesthetic carpules.10
There are three types of reactions to the wearing of gloves: nonimmunologic irritant contact dermatitis and two immunologic reactions—allergic contact dermatitis and latex allergy. The most common adverse reaction to wearing gloves is irritant contact dermatitis, which is a nonimmunologic irritation to nonlatex chemicals. The result is dry, reddened, itchy, and cracked skin. Frequent exposure to handwashing chemicals and incomplete rinsing and poor drying worsen the problem. Exposure to cornstarch and sweating exacerbate the irritation. Relief can occur through proper handwashing and perhaps by changing the type of glove and/or manufacturer.10
A discussion of immunological hypersensitivities, including allergic contact dermatitis and latex allergy, is beyond the scope of this article. However, a good review of the topic can be found in FirstHand, a publication of Kimberly-Clark Health Care Education, at http://latexallergyresources.org/sites/default/files/article-attachments/Safeskin-4.2.pdf.
Exposure to glutaraldehyde, hydrogen peroxide, and alcohol preparations may weaken latex, vinyl, nitrile, and other synthetic glove materials. Other chemicals commonly associated with dental care also may weaken gloves. Because of the diverse selection of dental materials on the market, glove users should consult the glove manufacturer about the compatibility of the glove material with various chemicals.12
Wearing gloves does not replace the need for handwashing. Personnel should wash and dry their hands well immediately before donning gloves. Gloves may have small, unapparent defects or may be torn during use, and hands can become contaminated during removal. Also, bacteria can multiply rapidly in the moist environment underneath gloves. Hands must be washed immediately after glove removal.10,12
Eye/Face Protection
Eye/face protection is often used in conjunction with other PPE such as gloves, gowns, masks, or respirators. Dental healthcare personnel should wear protective eyewear with solid side shields or a face shield during procedures, patient-care activities, clean-up, instrument reprocessing, and laboratory work. Protective eyewear protects the mucous membranes of the eyes from contact with microorganisms in splashes, sprays, and aerosols. Reusable protective eyewear should be cleaned with soap and water, and when visibly soiled, disinfected between patients.1,10,12,15
Goggles (safety glasses, lab glasses) provide the greatest level of eye protection, including impact, heat, and chemical resistance, plus protection from the front, top, and sides. Although they are typically unattractive, bulky, and heavy, goggles fit snuggly to the worker’s face and can be worn alone or over prescription spectacles.10,16
Many practitioners wear prescription spectacles (glasses). Spectacles must meet ANSI Z87.1 standards and, in particular, have adequate impact resistance.17 Spectacles are available with side shields attached or removal side shields that are disposable. The OSHA Bloodborne Pathogens Standard describes the performance abilities expected.1
Face shields are commonly used as an infection control alternative to goggles. Unlike goggles, a face shield can also provide protection to other facial areas. Face shields should offer forehead and chin protection and wrap around the face to the ears. This reduces the chances of fluids reaching facial skin or the eyes. Face shields should be sufficiently thick to stop projectiles and resistant to hazardous chemicals. Masks should also be used when wearing a face shield.10,18 Disposable face shields are made of lightweight films that are attached to a surgical mask fit loosely around the face and should not be relied upon for providing optimal protection.10,16
Protective eyewear can also be provided for patients to protect their eyes from spatter or debris generated during dental procedures. This can minimize injuries due to errant digits and instruments, projectiles, and hazardous chemicals. Several types of disposable eyewear are available, and reusable patient eyewear can be cleaned and disinfected before reuse.10,15
Table 2 provides a comparison of eye protection devices.10,16,17
Protective Clothing (Gowns)
Protective clothing (eg, gowns, jackets, and aprons) is worn to prevent contamination of street clothing and to protect the skin of personnel from exposure to blood and body fluids. Choosing protective clothing can be complicated and problematic. The process can be facilitated using the aforementioned reasonable, necessary, and appropriate questioning scheme.
A gown is worn as PPE when spatter and spray of blood, saliva, or other potentially infectious material is anticipated. Protective clothing should be changed daily or sooner if visibly soiled. Personnel should remove protective clothing before leaving the work area.12
Ideally, protective clothing should be fluid-resistant (but not fluid-proof), have long sleeves and high necks, and cover knees when sitting. Again, comfort is conducive to compliance. Consideration should be given to balancing fluid resistance capabilities and wearability (heat and moisture build-up).
Two basic forms of protective clothing are reusable and single-use disposable. The employer is responsible for providing protective clothing. OSHA’s Bloodborne Pathogens Standard prohibits employees from taking home protective clothing and linens for laundering. Rather, it is the employer’s responsibility to either launder protective clothing in-house or to send it out to a commercial laundry service.1,10,12
Disposable protective clothing is a convenient way to provide protection. Such covers have long sleeves, high necks, and sufficient length to cover knees. Used gowns are not considered as regulated medical waste and can be placed into a facility’s general waste stream.1,10,12
In many healthcare offices, employees wear only scrubs clinically. They are comfortable and colorful; however, scrubs are not protective clothing, as they are not highly fluid resistant (ie, they allow direct access to skin) and typically have short sleeves and open necks. Scrubs are also often worn outside clinical areas and even home, and it is not always clear who launders them and where.
Donning and Doffing
The skin and clothing of healthcare personnel can get contaminated during removal of PPE. This could contribute to dissemination of pathogens and it places personnel at risk for infection. In one study, contamination of the skin and regular clothing of healthcare personnel occurred frequently during removal of contaminated gloves or gowns because of improper removal technique and poor PPE design.19 Another study indicated that under usual conditions, about half of healthcare workers correctly removed their PPE and very few removed it in the correct order and disposed of it properly.20 The CDC has produced instructive material that demonstrates the sequence for donning and removing PPE (Figure 2 through Figure 4). Posters provide key instructions to reinforce safe practices and are intended to limit the spread of contamination. Much of the material presented is appropriate for dentistry.21
The donning sequence is: gowns, masks, eye protection, and, finally, gloves. The CDC series supports wearing long-sleeved gowns and then placing gloves over the wrists. Thus, the gloves are extended over the cuffs of the gowns, leaving no exposed skin.
The removal sequence is: gloves, eye protection, gowns, and then masks. The intent is to remove the most contaminated PPE first—gloves—and then the eye protection. Contamination of gowns is usually greater in the front, so it is best to open and remove them from the back side. Masks are removed last. After proper disposal of the PPE, hand hygiene should be performed.
Conclusion
PPE is designed to protect the skin and the mucous membranes of the eyes, nose, and mouth of dental personnel. OSHA mandates that dental personnel wear gloves, surgical masks, protective eyewear, and protective clothing when performing certain clinical and laboratory activities to reduce the risk of exposures to bloodborne pathogens and other occupational hazards.12
ABOUT THE AUTHOR
Charles John Palenik, MS, PhD, MBA
In 2011, Dr. Palenik retired after 35 years at Indiana University School of Dentistry, Indianapolis Indiana. He held a number of academic and administrative positions, including Professor of Oral Microbiology, Director/Human Health & Safety, Director/Central Sterilization Services, and Chairman/Infection Control and Hazardous Materials Management Committees. Currently, he is President and CEO of GC Infection Prevention and Control Consultants, Indianapolis, Indiana.
REFERENCES
1. About OSHA. US Dept of Labor – Occupational Safety and Health Administration website. https://www.osha.gov/about.html. Accessed April 10, 2017.
2. OSH Act of 1970. General Duty Clause. US Dept of Labor – Occupational Safety and Health Administration website. https://www.osha.gov/pls/oshaweb/owasrch.search_form?p_doc_type=OSHACT&p_toc_level=0&p_keyvalue=&p_status=CURRENT. Accessed April 10, 2017.
3. General Duty Clause - SEC. 5. Duties. US Dept of Labor – Occupational Safety and Health Administration website. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=OSHACT&p_id=3359. Accessed April 10, 2017.
4. Bloodborne Pathogens Standard. US Dept of Labor – Occupational Safety and Health Administration website. http://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=10051. Accessed April 10, 2017.
5. Hazard Communication Standard. US Dept of Labor – Occupational Safety and Health Administration website. https://www.osha.gov/dsg/hazcom/. Accessed April 10, 2017.
6. Ionizing Radiation Communication Standard. US Dept of Labor – Occupational Safety and Health Administration website. https://www.osha.gov/pls/oshaweb/owadisp.show_document?p_table=STANDARDS&p_id=10098. Accessed April 10, 2017.
7. Recommended practices for safety and health programs. US Dept of Labor – Occupational Safety and Health Administration website. https://www.osha.gov/shpguidelines/hazard-prevention.html#ai1. Accessed April 10, 2017.
8. Hierarchy of controls. Occupational Safety and Health Administration website. https://www.osha.gov/dte/grant_materials/fy10/sh-20839-10/hierarchy_of_controls.pdf. Accessed April 10 2017.
9. Centers for Disease Control and Prevention. Summary of Infection Prevention Practices in Dental Settings: Basic Expectations for Safe Care. Atlanta, GA: Centers for Disease Control and Prevention, US Dept of Health and Human Services; October 2016.
10. Miller CH. Infection Control and Management of Hazardous Materials for the Dental Team. 6th ed. St. Louis, MO: Elsevier; 2018.
11. Sanchez E. Filtration efficiency of surgical masks [master’s thesis]. Tampa, FL: Department of Environmental and Occupational Health, College of Public Health, University of South Florida; 2010.
12. Infection control. Frequently asked questions - personal protective equipment (masks, protective eyewear, protective apparel, gloves). Centers for Disease Control and Prevention website. https://www.cdc.gov/oralhealth/infectioncontrol/faq/protective_equipment.htm. Accessed April 10, 2017.
13. Food and Drug Administration. Banned Devices; Powdered Surgeon’s Gloves, Powdered Patient Examination Gloves, and Absorbable Powder for Lubricating a Surgeon’s Glove. Final rule. Fed Regist. 2016;81(243):91722-91731.
14. FDA bans use of powdered gloves. The Joint Commission Perspectives. March 2017; p.4. https://www.jointcommission.org/assets/1/18/FDA_Bans_Powdered_Gloves.pdf. Accessed April 10, 2017.
15. Eye safety. Centers for Disease Control and Prevention – National Institute for Occupational Safety and Health website. https://www.cdc.gov/niosh/topics/eye/eye-infectious.html. Accessed April 10, 2017.
16. Palenik CJ. Eye protection for dental laboratories. J Dent Technol. 1997;14(7):22-26.
17. American National Safety Institute. American National Standard for Occupational and Educational Personal Eye and Face Protection Devices - ANSI/ISEA Z87.1-2015. New York, NY, 015.
18. Palenik CJ. The “eyes” have it. RDH. 20013;23:69-70.
19. Tomas ME, Kundrapu S, Thota P, et al. Contamination of health care personnel during removal of personal protective equipment. JAMA Internal Med. 2015;175(12):1904-1910.
20. Zellmer C, Van Hoof S, Safdar N. Variation in health care worker removal of personal protective equipment. Am J Infect Control. 2015;43(7):750-751.
21. Donning and removing PPE. Centers for Disease Control and Prevention website. https://www.cdc.gov/hai/pdfs/ppe/PPE-Sequence.pdf. Accessed April 10, 2017.