You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
Tooth cracks are incomplete fractures without visible separation or mobility of the segments along the plane of the fracture.1 A complete fracture, on the other hand, involves separation or mobility of the segments, such as a split tooth or a fractured cusp.1 Tooth cracks can be symptomatic or asymptomatic. They can be vertical or oblique; vertical cracks extend toward the center of the tooth in mesiodistal and/or buccolingual directions, and oblique cracks extend under the cusps. Vertical cracks can either be seen in enamel only or also extend into dentin, and they are more likely than oblique cracks to propagate into underlying structures and render the tooth nonrestorable.2
Generally, cracks are addressed when they are symptomatic. Such cracks collectively are referred to as cracked tooth syndrome. If clinicians rely only on symptoms to initiate the process of diagnosing and treating cracks, however, the tooth and its surrounding structures may be put at risk of further damage, and more invasive treatment approaches may be required with the tooth even possibly being rendered unsavable. Asymptomatic cracks can be precursors to cracked tooth syndrome and complete fracture; thus, early recognition can help prevent further crack propagation.3 Of particular note is the significant increase in crack growth rates in deeper dentin due to increased tubular density, which warrants even earlier management.4
Having an understanding of the potential pathologic consequences of asymptomatic vertical cracks if no intervention is attempted, the capabilities and limitations of the available diagnostic tools, current conservative treatment approaches, and the challenges of early treatment of asymptomatic vertical cracks will help set the stage for clinicians to adopt a systematic approach for early diagnosis and intervention.
Pathologic Consequences
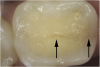
The detrimental effects of vertical cracks on the dentition and surrounding tissues stem mostly from bacterial invasion into the microscopic space of the crack, as well as physical irritation and liquid microleakage, even though the separation of the segments may not be clinically visible.3,5-7 As bacteria penetrate cracks, they invade underlying structures, such as the coronal dentin, pulp, root structure, and periodontal tissues, leading to varying degrees of pathologies. Enamel cracks have been found to provide caries-producing bacteria access to the dentin-enamel junction, leading to caries inside the tooth without any externally visible evidence (Figure 1).5 Dentin cracks are pathways of bacteria to the dentinal tubules and pulp, leading to various pulpal pathologies, including reversible and irreversible pulpitis and pulp necrosis.6,8
As cracks extend subgingivally along the root surface into the periodontal attachment, they create an open pathway of irritants, including bacteria from the oral cavity and from involved root canal spaces to the reactive periodontium, causing inflammation of the periodontium and bone loss along the fracture line.7 Cracks are precursors to complete fractures, and, if permitted to progress to their natural conclusion, they can render teeth unsalvageable.2,3 Although they do not occur nearly as frequently as caries and periodontal disease, tooth fractures are still the third-most common cause of tooth loss and can appear in dentitions that are well cared for and maintained.9 These pathologic consequences are an impetus to address asymptomatic vertical cracks at very early stages.
Diagnosis
The diagnosis of asymptomatic vertical cracks can be an integral part of the comprehensive evaluation of the dentition; such cracks could be actively sought out instead of accidentally discovered.
Scant literature is available regarding the incidence of asymptomatic cracks in the general population. In 51 patients examined, Ratcliff and coworkers10 reported a 33.71% incidence of stained and unstained asymptomatic cracks in posterior teeth with and without restoration. In a Northwest Dental Practice-Based Research Network study, 70% of 400 randomly selected subjects had at least one posterior cracked tooth, and 93% of these were asymptomatic.11 Other authors have advised that as an increasing number of patients retain more teeth into older age the incidence of cracks will rise in the future.12 Although the majority of cracks seen in restored teeth extend mesiodistally, 2,13,14 all surfaces and non-restored teeth should be inspected closely. In one study it was reported that, in the absence of restorations, caries, or luxation injuries, all 27 teeth diagnosed with pulp necrosis were found to have a longitudinal fracture extending from the occlusal surface into the pulp.8 Additionally, other studies reported 28% to 48.6% of diagnosed cracks were found in non-restored teeth.15,16
Asymptomatic enamel and dentin cracks may not always be readily apparent and can be difficult to diagnose, especially at their preliminary stages. However, they can usually still be detected by magnification, tactile examination, transillumination, or staining with dyes.
Magnification
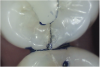
Magnification is the key element for initial assessment of cracks in their early stages and for integrating crack diagnosis into routine dental examination (Figure 2).2,6,8,12,14-18 The diagnosis process starts with careful visual inspection of the absolutely dried tooth. Although dental microscopes are ideal magnification tools, magnifying loupes with headlight illumination can provide considerable magnification when compared with unaided vision. The author used 4.8x magnifying loupes with coaxially mounted headlight illumination of 7,000 foot-candle of light output in the diagnosis and treatment of the cracks presented in this article.
Intraoral photography is another highly valuable diagnostic magnification tool that has the additional benefits of crack co-diagnosis and patient education. Magnification is, thus, the primary tool to use to draw one’s attention to suspicious areas requiring further investigation.
Tactile Examination
Cracks can be evaluated tactilely using a sharp explorer.10,17,19 Sharp explorers can be used to detect gaps up to 36-μm wide.20 The tip of a sharp explorer is passed along the tooth surface and “catches” a crack to help assess the severity of enamel cracks.17
Transillumination
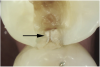
The use of fiber-optic transillumination for crack diagnosis is well documented in the literature.1-3,5,6,8-10,12,15-17,21-23 Teeth with significant cracks transilluminated with a fiber-optic light source will show a well-defined demarcation of blocked illumination at the crack lines, whereas structurally sound teeth will dissipate the light gradually throughout the tooth structure (Figure 3).22 While a variety of transillumination devices have been used to reveal cracks, pen-sized cordless units with a highly collimated light source and that are specifically manufactured for this purpose are ideal for this diagnostic technique. This is mainly because they emit the proper amount of light intensity to highlight cracks, and viewing can be done directly with the eye without using a protective device.22
Staining
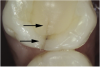
Methylene blue dye is the most commonly used dye to stain cracks because of its pooling tendency.2,3,14,16,17,23 The dye pools into the enamel and dentin cracks and the tooth is thoroughly rinsed. The resulting dark stain retained in the crack lines then helps enable cracks to be detected (Figure 4 and Figure 5). Methylene blue dye, however, also stains dental plaque, requiring the tooth surface to be cleaned with pumice or prophylaxis paste before dye application.14 The dye also can be absorbed by dentin, but any residual dye can be removed using a 10-second phosphoric acid etch.14 A comparative study of dye staining and transillumination concluded that methylene blue dye staining and transillumination performed simultaneously is the optimal crack assessment technique.23
Treatment Considerations
Similar to diagnosis, the treatment of asymptomatic cracks can be incorporated into the comprehensive treatment of the dentition. Treatment begins by evaluating and treating asymptomatic vertical enamel cracks. In a recent study in which intraoral images of enamel cracks were projected on a screen to ensure the uniformity of referenced cases, 80% of the 51 participating general dentists indicated they would recommend treatment for asymptomatic enamel cracks.19 However, which enamel cracks are considered significant, requiring intervention, and which are less significant, requiring only monitoring and preventive measures, is still not clearly standardized. Monitoring should be used with caution because 27% of cracked teeth observed in the aforementioned Northwest Dental Practice-Based Research Network study showed progression in just 1 year.11 This is primarily due to the complex and multifactorial etiology of cracks that weakens tooth structure, such as large cavity preparations and incomplete developmental fusion of areas of calcification, as well as exertion of damaging forces on teeth from such sources as horizontal occlusal forces, bruxism, and masticatory accidents.24
Asymptomatic vertical enamel cracks that are both naturally stained and detectable by an explorer are more likely to be treated than asymptomatic cracks that are only detectable by transillumination and dyes.19 Intervention has also been recommended for moderate- to high-risk enamel cracks, such as cracks with wedge-shaped enamel ditching, cracks that either detour from or do not follow anatomic grooves, pairs of cracks that outline an area of discolored enamel, cracks that house debris, and cracks with a brown, gray, or white corresponding halo.14
Once a significant asymptomatic enamel crack is diagnosed, to determine its extent the crack is exposed and traced using a minimally invasive exploratory fissurotomy as well as caries removal and/or existing restoration removal whenever indicated (Figure 6 and Figure 7).2,3,17 If the crack is limited to enamel and does not extend into dentin, it can be completely eliminated and treated similarly to caries whereby the condition of the remaining tooth structure dictates the type of the restoration placed and the materials used (Figure 8). For example, moderate-sized cavity preparations can support bonded direct intracoronal resin-based composite restorations (Figure 9).25 This is generally interpreted as cavity preparations in which the isthmus width is less than 50% of the intercuspal distance and the remaining enamel is sound and well supported by dentin. Occlusal adjustment, including removal of excursive interferences, might also be necessary to eliminate localized heavy occlusal forces that are predisposing the tooth to cracking.10,19,26 Occlusal guards also can be fabricated to protect teeth from the damage caused by ongoing bruxism.19
Whenever asymptomatic enamel cracks extend into dentin and cannot be eliminated by minimally invasive fissurotomy without causing additional damage to the tooth and underlying structures, protection is recommended to minimize their propagation (Figure 10 and Figure 11).3,14 Occlusal coverage restorations have demonstrated greater overall success in the treatment of symptomatic cracks by immobilizing the cracked segments that move on loading, with better prognosis seen when more conservative restorations are used.27,28 Although this might still be controversial, from a biomechanical perspective these principles can conceptually apply to the treatment of asymptomatic dentin cracks. Occlusal coverage restorations have been recommended to protect asymptomatic teeth with existing dentin cracks from further cracking (Figure 12).2,3,9,29
In a study in which intraoral images of dentin cracks were projected on a screen to ensure the uniformity of referenced cases, 74% of the 47 participating general dentists who treat asymptomatic dentin cracks recommended occlusal coverage restorations for both stained and unstained asymptomatic vertical dentin cracks.19 The choice of dental materials and the specific designs of occlusal coverage restorations used in the treatment of asymptomatic dentin cracks depend on each tooth’s additional needs, the clinician’s preferences, and the specific functional and esthetic needs of each patient, as long as the aforementioned objective of immobilizing the cracked segments of the tooth on loading is achieved. However, cracks can still propagate under restorations due to their multifactorial etiology, as described earlier. Thus, placing bonded occlusal coverage restorations with a ferrule effect and reducing occlusal stresses, along with early intervention, will help to ensure better long-term treatment outcome.
Challenges of Asymptomatic Crack Management
Clinicians face many challenges when managing asymptomatic cracks in their early stages. Limited evidence is available in the current literature addressing the management of asymptomatic cracks; in particular, there is a lack of longitudinal studies comparing the available approaches of protective intervention versus monitoring for the various forms of asymptomatic cracks. This lack of definitive information forces dentists to rely mostly on their own individual experience and differing expert opinions. Currently, the literature evaluates various restorative approaches, such as bonded direct and indirect intracoronal restorations and different occlusal coverage restorations, in terms of their effect on the fracture resistance of teeth weakened by wide cavity preparations and for the treatment and prevention of symptomatic cracks, but not specifically for teeth with already existing asymptomatic dentin cracks regardless of cavity preparation size.27,30 This leads to controversy regarding both the necessity and the most appropriate modes of protective intervention for teeth with asymptomatic cracks to limit their propagation.31
The current diagnostic tools cannot determine the full extent of cracks without intervention, and significant enamel cracks do not always indicate the presence of underlying dentin cracks.2,14 A definitive treatment plan for the type of final restoration, especially in the case of occlusal coverage restorations, generally cannot be made preoperatively based on the initial clinical impression of the enamel crack if the tooth is otherwise not compromised except for the enamel crack. An exploratory fissurotomy and/or removal of the existing restoration and caries is still needed first to verify the extent of the enamel crack and determine the condition of the remaining tooth structure.
Additionally, it is questionable as to whether or not preoperative thermal and electric pulp vitality assessment is needed to rule out asymptomatic pulp necrosis that could have resulted from a possible underlying deep dentin crack in teeth with asymptomatic enamel cracks if these teeth have not demonstrated any preoperative clinical or radiographic evidence of pulpal pathology. Preoperative pulp vitality testing might be preferred for several reasons: pulp vitality of an anesthetized tooth cannot be assessed intraoperatively after fissurotomy has revealed deep dentin cracks; deep dentin cracks cannot always be conservatively explored to determine their precise proximity to the pulp without risking further damage; and the option of assessing pulp vitality while the tooth has a temporary restoration is becoming less feasible as single-visit CAD/CAM indirect restorations become more prevalent. Preoperative pulp vitality testing, however, might not necessarily be clinically as crucial because the chances of pulp necrosis decrease considerably when asymptomatic cracks are treated preventively at earlier stages; consequently, pulp vitality testing is not likely to reveal a significant number of necrotic teeth. Regardless, periodic clinical and radiographic pulpal monitoring is still advised because dentin cracks can still propagate under occlusal coverage restorations.
Overcoming the challenges of managing asymptomatic vertical cracks at their early stages requires a paradigm shift in the way they are viewed. Several initial steps can be taken to incorporate early diagnosis and treatment of asymptomatic cracks into daily practice. First, clinicians should become familiar with the clinical presentations of the various forms of asymptomatic vertical enamel and dentin cracks and their significance in terms of the risks of pathologic consequences they impose on the dentition and surrounding structures when intervention is postponed. Additionally, multiple diagnostic tools, especially light-assisted magnification, should be used, and clinicians should employ visual educational tools to help educate and guide patients to make informed decisions. Further steps include adopting conservative treatment approaches, always starting with a conservative exploratory fissurotomy and/or caries and restoration removal; monitoring teeth and their surrounding structures periodically after treatment; and knowing the limitation of the current evidence and actively looking for emerging evidence.
Conclusion
Delaying intervention of asymptomatic vertical enamel and dentin cracks can result in various pathologic consequences, which can range from caries to pulpal and/or periodontal involvement, total tooth fracture, and potential tooth loss. Diagnosis should be done in early stages using a variety of methods, including magnification, tactile examination, transillumination, and dyes, and treatment of asymptomatic cracks can be integrated into the comprehensive care of a patient’s dentition. By incorporating early restorative and occlusal treatments into daily practice, clinicians can prevent further crack propagation before asymptomatic cracks become symptomatic and cause further damage to the dentition and surrounding tissues.
About the Author
Samer S. Alassaad, DDS
Private Practice
Davis, California
Fellow
Academy of General Dentistry
Queries to the author regarding this course may be submitted to authorqueries@aegiscomm.com.
References
1. Luebke RG. Vertical crown-root fractures in posterior teeth. Dent Clinic North Am. 1984;28(4):883-894.
2. Ailor JE Jr. Managing incomplete tooth fractures. J Am Dent Assoc. 2000;131(8):1168-1174.
3. Abou-Rass M. Crack lines: the precursors of tooth fractures – their diagnosis and treatment. Quintessence Int Dent Dig. 1983;14(4):437-447.
4. Ivancik J, Neerchal NK, Romberg E, Arola D. The reduction in fatigue crack growth resistance of dentin with depth. J Dent Res. 2011;90(8):1031-1036.
5. Walker BN, Makinson OF, Peters MC. Enamel cracks. The role of enamel lamellae in caries initiation. Aust Dent J. 1998;43:(2):110-116.
6. Ricucci D, Siqueira JF Jr, Loghin S, Berman LH. The cracked tooth: histopathologic and histobacteriologic aspects. J Endod. 2015;41(3):343-352.
7. Walton RE, Michelich RJ, Smith GN. The histopathogenesis of vertical root fractures. J Endod. 1984;10(2):48-56.
8. Berman LH, Kuttler S. Fracture necrosis: diagnosis, prognosis assessment, and treatment recommendations. J Endod. 2010;36(3):442-446.
9. Braly BV, Maxwell EH. Potential for tooth fracture in restorative dentistry. J Prosthet Dent. 1981;45(4):411-414.
10. Ratcliff S, Becker IM, Quinn L. Type and incidence of cracks in posterior teeth. J Prosthet Dent. 2001:86(2):168-172.
11. Northwest PRECEDENT: Assessing Outcomes of Cracked Teeth. National Institute of Dental and Craniofacial Research website. Updated February 26, 2014. http://nidcr.nih.gov/Research/DER/ClinicalResearch/PBRNStudyHighlights.htm. Accessed September 27, 2017.
12. Banerji S, Mehta SB, Millar BJ. Cracked tooth syndrome. Part 1: aetiology and diagnosis. Br Dent J. 2010;208(10):459-463.
13. Cameron CE. The cracked tooth syndrome: additional findings. J Am Dent Assoc. 1976;93(5):971-975.
14. Clark DJ, Sheets CG, Paquette JM. Definitive diagnosis of early enamel and dentin cracks based on microscopic evaluation. J Esthet Restor Dent. 2003;15(7):391-401.
15. Seo DG, Yi YA, Shin SJ, Park JW. Analysis of factors associated with cracked teeth. J Endod. 2012;38(3):288-292.
16. Kim SY, Kim SH, Cho SB, et al. Different treatment protocols for different pulpal and periapical diagnoses of 72 cracked teeth. J Endod. 2013;39(4):449-452.
17. American Association of Endodontists. The obvious and the obscure: steps for crack detection and confirmation. Endodontics: Colleagues for Excellence Newsletter. 2008. http://www.aae.org/uploadedFiles/Publications_and_Research/Endodontics_Colleagues_for_Excellence_Newsletter/LTFBonusMaterial_C.pdf. Accessed September 27, 2017.
18. Mamoun JS. A rationale for the use of high-powered magnification or microscopes in general dentistry. Gen Dent. 2009;57(1):18-26.
19. Alassaad SS. Approaches to managing asymptomatic enamel and dentin cracks. Gen Dent. 2014;62(6):58-62.
20. Baldissara P, Baldissara S, Scotti R. Reliability of tactile perception using sharp and dull explorers in marginal opening identification. Int J Prosthodont. 1998;11(6):591-594.
21. Liewehr FR. An inexpensive device for transillumination. J Endod. 2001;27(2):130-131.
22. Alassaad SS. Incomplete cusp fractures: early diagnosis and communication with patients using fiber-optic transillumination and intraoral photography. Gen Dent. 2011;59(2):132-135.
23. Wright HM Jr, Loushine RJ, Weller RN, et al. Identification of resected root-end dentinal cracks: a comparative study of transillumination and dyes. J Endod. 2004;30(10):712-715.
24. Lynch CD, McConnell RJ. The cracked tooth syndrome. J Can Dent Assoc. 2002;68(8):470-475.
25. Statement on posterior resin-based composites. ADA Council on Scientific Affairs; ADA Council on Dental Benefit Programs. J Am Dent Assoc. 1998;129(11):1627-1628.
26. Agar JR, Weller RN. Occlusal adjustment for initial treatment and prevention of the cracked tooth syndrome. J Prosthet Dent. 1988;60(2):145-147.
27. Banerji S, Mehta SB, Millar BJ. Cracked tooth syndrome. Part 2: restorative options for the management of cracked tooth syndrome. Br Dent J. 2010;208(11):503-514.
28. Opdam NJ, Roeters JJ, Loomans BA, Bronkhorst EM. Seven-year clinical evaluation of painful cracked teeth restored with a direct composite restoration. J Endod. 2008;34(7):808-811.
29. Christensen GJ. When is a full-crown restoration indicated? J Am Dent Assoc. 2007;138(1):101-103.
30. Geurtsen W, García-Godoy F. Bonded restorations for the prevention and treatment of the cracked-tooth syndrome. Am J Dent. 1999;12(6):266-270.
31. Lubisich EB, Hilton TJ, Ferracane J; Northwest Precedent. Cracked teeth: a review of the literature. J Esthet Restor Dent. 2010;22(3):158-167.