You must be signed in to read the rest of this article.
Registration on CDEWorld is free. You may also login to CDEWorld with your DentalAegis.com account.
A thorough working knowledge of the fundamentals of occlusion and jaw function is critical to the management of patients in a general practice. That includes the differential diagnosis of pain, treatment planning, as well as the management of all types of occlusal disease. It also includes a global way of thinking about occlusion. In other words, what is the role of occlusion in everyday practice?
Occlusion and designing an occlusal scheme is about managing force. It is the repetitive application of forces that exceed the patient’s capacity to tolerate those forces that leads to damage, disease, and dysfunction. Occlusal disease is manifested as different types of structural damage including wear, fractures, and restorative material failure. It also includes tooth mobility, gingiva and bone loss, muscle pain, joint pain and noises (ie, clicking), limitations and deviations of mandibular movement, as well as remodeling of the articulating components of the joints. In extreme cases, the bony remodeling can lead to degenerative joint disease.1 The forces that exceed normal function are generated in parafunctional habits of which the patient is often unaware. Generally, we can observe and measure the signs and the results of the repetitive application of forces to and by these tissues and restorative materials.
To add to the complexity of this subject is what the published literature says regarding the relationship between occlusion and temporomandibular disorders. The large-scale literature reviews find little association between occlusion and temporomandibular disorders.2-4 Furthermore, they do not find a high association between occlusal correction and improvement or prevention of these disorders. What can be concluded from this and clinical practice is this: Absent traumatic injuries, if a patient does not apply force to their functional system that exceeds their capacity to tolerate it, then disease and dysfunction will not be present—or it will not be present to a significant degree. That statement holds true regardless of how ideal, or not ideal, their occlusal scheme is.
However, when a patient applies excessive forces repetitively over longer periods of time, then occlusal disease and dysfunction occur, regardless of the occlusal scheme. Differing types of malocclusion exacerbate the disease and dysfunction. What that means is that when clinicians begin to understand the impact of occlusal schemes and conditions on teeth, restorations, gingiva, bone, muscles, and joints, then they can design a scheme that is much more stable, much less damaging, and much more functional for the patient. In other words, the fundamentals of occlusion can give clinicians a way to think, plan, and execute that plan of restoring the damage that is all too often found in patients that have suffered significant functional disease. The elephant in the room of temporomandibular joint disorders, occlusion, and functional disease is force—repetitive force that exceeds the patient’s capacity to adapt. This author does not believe that it is reasonable to separate the dynamics of force application to human tissue and the disease and dysfunction experienced by that same tissue. In his view, the better question to ask is the relationship between parafunction, occlusion, and functional disease.
Foundational to understanding jaw function and occlusion is the anatomy of the muscles of mastication, the temporomandibular joint, and of course the teeth. Then building on this understanding of the anatomy, there needs to be a way to think about the relationship between the mandible and the maxilla. Next, what is desirable in both static tooth contacts and dynamic tooth contacts during mandibular movement needs to be determined. Finally, how should these principles of occlusion be integrated into a treatment plan designed to correct structural damage to a patient’s teeth and the resulting esthetic problems, as well as create stability and comfort?
In reviewing anatomy, tooth relationships, and jaw relationships, clinicians should look for reference points to guide their understanding and decision-making. Occlusion is integral to and inseparable from comprehensive treatment planning. In this article, the author will reference the concepts of facially generated treatment planning as developed and taught by Dr. Frank Spear. In cases where teeth have suffered extensive damage resulting in significant dentoalveolar compensation, the typical reference points are lost. To restore patients to proper function, health, esthetics, and stability, clinicians need a way to properly reestablish those reference points. Facially generated treatment planning provides a framework to do just that.
Pankey’s Rules of Optimum Occlusion
Dr. L. D. Pankey, a pioneer and master in complex oral rehabilitation, gave clinical dentistry a great way to think about the role of occlusion in both complex rehabilitations and everyday dental treatment.
• With the condyles fully seated in the fossa, all the posterior teeth touch simultaneously and evenly, with the anterior teeth lightly touching.
• When the patient squeezes, neither a tooth nor the mandible moves..
• When the mandible is moved in any excursion, no back tooth hits before, harder than, or after a front tooth.5
• With those goals in mind, it is time to look at the anatomy of jaw function.
Anatomy of the Temporomandibular Joint
In Figure 1, the condyle of the mandible can be seen in a very intimate relationship with a biconcave disc. This is all contained in a capsule that is secured posteriorly by the retrodiscal attachments and inferiorly by the capsular attachment to the neck of the condyle. Anteriorly, the superior head of the lateral pterygoid muscle is seen attaching to both the disc and the neck of the condyle while the inferior head attaches only to the neck of the condyle.6 Posterior to the joint is the external auditory meatus. Anterior and superior to the condyle is the eminence. Directly superior is the glenoid fossa. The articulating surfaces are covered in fibrocartilage that is very smooth and supported by synovial fluid that lubricates the articulating surfaces, provides nutrients and oxygenation, as well as removing debris. There is very limited to no blood supply within the joint capsule.
Examination of the joint components reveals several observations that are critical. First is the intimate relationship of the condyle/disc/fossa assembly. Essentially, they are in the most closely packed arrangement that is possible for them.7 This arrangement allows the temporomandibular joint to be a load-bearing joint. It also allows for dynamic movements of the mandible while maintaining the anatomical relationship of the condyle/disc assembly as it moves out of the fossa and down the eminence. Later, we will observe that in certain types of joint disorders, that relationship is disrupted.
Obviously, there is great variation of the size, volume, and shape of the anatomical features of the joints from person to person. Historically, we viewed the dimensions of the condyle as being relatively fixed. However, recent investigations have established that the dimensions of the condyle can change and adapt over time as the demands on the joint change.8,9 As a very distinct example, sleep appliances that advance the mandible to open a patient’s airway appear to stimulate bone growth in the condyle that is permanent. Therefore, it appears that the condyle has the capacity to adapt to functional requirements by remodeling as well as growing. It is clearly not as fixed in dimension as once was thought.
Determining and recording the position of the condyle is the first critical reference point to establish. When possible, the centric relation (CR) position of the condyle serves as the most desirable treatment position.10-12
CR has many desirable qualities in the rehabilitation of dental function. With excellent technique, patience, and effort, it can be precisely located with great confidence. It is a repeatable position that can be located and recorded regardless of the changes in tooth position or contact. In a stable joint, it has the greatest capacity to bear force. It allows the lateral pterygoid muscle to be passive during heavy clenching (Figure 2 and Figure 3).
Anatomy of the Muscles of Mastication
There are three muscles of mastication that elevate the mandible. These three closing muscles can generate significant amounts of force in clenching and bruxing.
First, the masseter muscle originates on the zygomatic arch and inserts into the inferior border of the mandible laterally. The vector of force produced is superior and anterior. The cross-sectional thickness of the masseter is a reasonable gauge of the amount of force that it can produce. It is positioned anterior to the temporomandibular joint.
Second, the temporalis muscle arises from the temporal fossa and the deep part of the temporal fascia. It passes medial to the zygomatic arch and forms a tendon that inserts onto the coronoid process of the mandible, with its insertion extending into the retromolar fossa posterior to the most distal mandibular molar. As its origin is a fan shape, the force vectors diverge. The anterior portion goes superiorly and slightly anteriorly, while the posterior portion runs superiorly and posteriorly. This becomes more important in the diagnosis of the conditions producing pain in different parts of this particular muscle.
Third, the medial pterygoid muscle consists of two heads. The bulk of the muscle arises just above the medial surface of the lateral pterygoid plate. The superficial head originates from the maxillary tuberosity and the pyramidal process of the palatine bone. Its fibers pass downward, laterally, and posteriorly, and are inserted, by a tendon, into the lower and posterior part of the medial surface of the ramus and angle of the mandible. The insertion joins the masseter muscle to form a common tendinous sling that allows the medial pterygoid and masseter to be powerful elevators of the jaw.7
There are several factors that make understanding these anatomical features important. First, the force vectors of all three muscles result in the condyle being seated superiorly in the glenoid fossa, anteriorly and superiorly against the eminence, and medially so that the medial pole is the most load-bearing aspect of the condyle. In other words, outside of the influence of tooth contacts, these three muscles will seat the condyle into the most superior position possible that is at the same time the most closely packed and intimate arrangement of the condyle disc fossa assembly.13
The digastric muscle is one of the main depressor muscles that open the mandible. It originates in the mastoid notch, passes through a tendinous sling midway, and inserts on the inferior border of the mandible near the symphysis in the digastric fossa. As an opening muscle, it is much more unusual for this muscle to exhibit pain.
The lateral pterygoid muscle moves the mandible laterally and forward. The superior head originates in the infra-temporal wing of the sphenoid bone. The inferior head originates from the lateral pterygoid plate. The muscle inserts via two parts into the neck of the condyle and the disc. Part of its function is to coordinate the disc position with the condyle to maintain a desirable functional relationship of the condyle disc assembly. Often, the lateral pterygoid muscle bears the burden of bracing the mandible in an eccentric position during periods of heavy clenching or bruxing when the existing tooth contacts require a deflection of the mandible to achieve maximum intercuspation. The three elevator muscles are much larger and exert much more force than the lateral pterygoid. Under these circumstances, the lateral pterygoid muscle will be required to contract way past its capacity to bear and produce sufficient force to antagonize the three elevator muscles. If it is required to do so, then it will likely become painful and possibly exhibit spasms.
Posterior Tooth Relationships
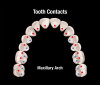
The first of Pankey’s three rules for occlusion is that all posterior teeth contact simultaneously when both condyles are in the fully seated CR position, as the anterior teeth contact equally or slightly less (Figure 4 and Figure 5). Essentially, every type of occlusal scheme, regardless of how the condylar position is determined, views simultaneous contact of all teeth as desirable. There are multiple benefits to this. First, the bite force is distributed more evenly over more teeth. Second, the lateral pterygoid muscles are not required to move or hold the mandible in an eccentric position. Third, an occlusal scheme of cusps contacting flat landing pads simultaneously with room around the inclines of the cusps will place forces down the long axis of the tooth without deflective lateral forces (Figure 6). Those deflective lateral forces can be responsible for various kinds of damage to teeth, restorations, gingiva, and bone. Finally, posterior teeth share the functional force generated by elevator muscles with both joints. With incisor-only contact, 60% of elevator muscle force is applied to the joints.14,15 With second molar contact, only 5% of the force is applied to the joints.14,15 In painful and unstable joints, it is critical to support them with abundant posterior tooth contacts.
Examination of the Functional System
An examination is a process of discovery that is focused on the patient’s conditions. The discovery begins in a “conversation that counts” with the patient prior to an examination. The idea of co-discovery was developed by another pioneer in preventive dentistry, Dr. Bob Barkley and expanded by Pankey.5,16 Barkley said that the best experience for the patient and the dental team was to share in the discovery of the patient’s conditions together.16 Therefore, in that conversation prior to the functional examination, taking a thoughtful and complete history is essential and foundational. The examination outline that follows here is a thorough and detailed assessment of the patient’s functional system. Dr. M. William Lockard outlines a very thorough and comprehensive approach to patient care in his book, “The Exceptional Dental Practice.”17
The functional examination includes a thorough assessment of the:
• Temporomandibular joints
• Muscles of mastication
• Range and character of movement of the mandible
• Static and dynamic tooth contacts
The global objective of a functional examination is to gather an abundant amount of the essential data to determine if the patient’s functional system is stable or unstable. If it is unstable, then the objective is to specifically pinpoint what structural damage, disease, or dysfunction has occurred. It is critical to complete the examination of all of the patient’s conditions before rendering a diagnosis. This requires discipline and intention. Often, some of the most critical information comes at the end of the functional examination or between the examination appointment and the consultation appointment, as the patient can continue discovery on their own and the dentist can continue discovery with the patient’s records.
The order of the examination process is up to the individual clinician. What is presented in this article is the sequence that the author has developed in his own private practice. First in the sequence is joint assessment. The goal of this step is to determine the following:
• Is there pain to palpation of the joints? If so, what is the character and severity?
• Are there joint noises on movement? If so, at what point of movement and what is the character of the sound? Is it painful?
• Does the mandible move freely and without restriction? Does it deviate? If yes, how much and which direction?
• Can the joints tolerate force or load?
Positioning yourself at the 12 o’clock position allows the examiner to look down the long axis of the patient’s head for deviations of movement and symmetry. In adults, a full opening will be more than 40 mm. Many people will open past 50 mm. Likewise, normal lateral movement of the mandible is around 10 mm or so. Is there pain on lateral movement? Is the lateral range of motion different on one side or another? Movement of the mandible will be determined by the condyle/disc/fossa/eminence assembly and the stability of the lateral pterygoid muscles as well as the opening muscles. The most damaged or unstable joint will move less freely than the more stable side. With this initial joint and range of motion assessment, a pattern begins to emerge.
Critical in the examination is locating and recording the CR position of the condyle. The author uses bimanual guidance as developed by Dawson,18 as well as a leaf gauge, and a Lucia Jig that are different versions of an anterior stop.19 An anterior stop with no posterior contacts allows the elevator muscles to seat the condyles superiorly until the disc/fossa assembly stops it. Using anterior stops is a very reliable method to locate CR. The patient is asked to protrude, and this is retried multiple times on the anterior stop followed by clenching to activate the elevator muscles. The initial attempts to locate CR may be impaired by disc derangement, swelling with fluid within the capsule, and spasms in the lateral pterygoid muscles. So, initially the examiner may only be able to locate a tentative CR position. As the joints and muscles stabilize, a more refined and accurate location will unfold.
Using the same three methods of locating CR, the examiner can test the capacity of the joints to tolerate force. In other words, is the condyle/disc/fossa assembly stable and healthy enough to bear the force of normal function and parafunction? In a very basic sense, the possible conditions that could contribute to instability include joint inflammation, disc derangement, disruption of the articulating surfaces, and pain in the attachment of the lateral pterygoid muscle into the condyle and disc. By having the patient repeatedly make protrusive and retrusive movements on the leaf gauge and/or the Lucia Jig, followed by clenching, both the joint and the lateral pterygoid muscle get tested. In a like manner, increasing the superior force applied in bimanual guidance is a great way to load-test the joints.
Next in the examination are the muscles. This can be as detailed or as basic as the clinician desires. This part of the examination is to determine the following:
• The status of the three elevator muscles. Is there discomfort to palpation? What is the cross-sectional thickness? How much tension is present? How does the patient respond to my palpation?
• The status of the lateral pterygoid muscles. Mainly, is there pain to palpation or provocation?
• The status of the opening muscles in the floor of the mouth.
• The status of the muscles in the neck and shoulders.
The palpation of each of these muscles is different, but accessing as much of the muscle as is available is desirable. Start gently and increase pressure slowly while observing the patient’s response because this is very revealing, especially the visible response in their eyes. Again, grade their pain response as 1-2-3 for mild-moderate-severe. The author also makes note of the relative cross-sectional thickness of the masseter and the temporalis. The cross-sectional thickness of these two elevator muscles is a very reliable indicator of the patient’s capacity to generate force during clenching or bruxing. As a general observation, a patient with a low angle mandible builds thicker masseter muscles and, as such, will generate more force.
Finally, determining which teeth contact in various jaw relationships is critical to understanding the patient’s condition. First, determining the first tooth contact in CR is a critical reference point, even if the patient is not treated to a CR position. The author will use both bimanual guidance and a leaf gauge to determine this position. Giving this part of the examination a little extra time can yield completely different results. Using either a Lucia Jig to deprogram the patient’s muscles of mastication and following with bimanual guidance or using a leaf gauge with the patient progressing leaf by leaf to evaluate the superior movement of the condyle into the fossa and the resulting first point of contact can be a critical discovery for the examiner. It can give the clinician an idea of the vertical and horizontal adjustment necessary for the mandible to move into maximum tooth contact. That adjustment can require dramatically differing therapies to correct. It can also lead the clinician to determine that the correction is more involved than the benefit of the correction.
Conclusion
The anatomy of joints, muscles, and teeth and their relationships to one another provide the foundation for understanding dental occlusion and jaw function. This understanding is critical to managing patients every day and helping them to solve the clinical problems with which they present in a general practice. The forces generated in function and especially parafunction are the key to both the diagnosis and correction of clinical problems related to occlusion. A subsequent article will address anterior tooth relationships and the dynamics of mandibular movement in occlusal disease and dysfunction, especially wear. Also, the concepts of facially generated treatment planning will be incorporated into designing occlusal schemes that help to reduce the destructive impact of force on the entire functional system.
Disclosure
The author has no financial relationships to disclose.
References
1. Israel HA, Diamond B, Saed-Nejad F, Ratcliffe A. The relationship between parafunctional masticatory activity and arthroscopically diagnosed temporomandibular joint pathology. J Oral Maxillofac Surg. 1999;57:1034-1039.
2. Türp JC, Schindler H. The dental occlusion as a suspected cause for TMDs: epidemiological and etiological considerations. J Oral Rehabil. 2012;39: 502-512.
3. Koh H, Robinson PG. Occlusal adjustment for treating and preventing temporomandibular joint disorders. Cochrane Database Syst Rev. 2003;(1):CD003812.
4. Koh H, Robinson PG. Occlusal adjustment for treating and preventing temporomandibular joint disorders. J Oral Rehabil. 2004;31:287-292.
5. Mahan PE, Wilkinson TM, Gibbs CH, et al. Superior and inferior bellies of the lateral pterygoid muscle EMG activity at basic jaw positions. J Prosthet Dent. 1983;50:710-718.
6. Liu MQ, Chen HM, Yap AU, Fu KY. Condylar remodeling accompanying splint therapy: a cone-beam computerized tomography study of patients with temporomandibular joint disk displacement. Oral Surg Oral Med Oral Pathol Oral Radiol. 2012;114(2):259-265.
7. Hiyama S, Ono PT, Ishiwata Y, et al. Neuromuscular and Skeletal Adaptations Following Mandibular Forward Positioning Induced by the Herbst Appliance. Angle Orthod. 2000;70(6):442-453.
8. Dawson PE. Optimum TMJ condyle position in clinical practice. Int J Periodontics Restorative Dent. 1985;5:10-31.
9. Dawson PE. A classification system for occlusions that relates maximal intercuspation to the position and condition of the temporomandibular joints. J Prosthet Dent. 1996;75:60-66.
10. Dawson PE. New definition for relating occlusion to varying conditions of the temporomandibular joint. J Prosthet Dent. 1995;74:619-627.
11. Hannam AG, De Cou RE, Scott JD, Wood WW. The relationship between dental occlusion, muscle activity and associated jaw movement in man. Arch Oral Biol. 1977;22(1):25-32.
12. Ingawale SM, Goswami T. Biomechanics of the temporomandibular joint. In: Human Musculoskeletal Biomechanics, Goswami T (ed.). http://www.intechopen.com/books/human-musculoskeletal-biomechanics/biomechanics-of-the-temporomandibular-joint. Accessed September 26, 2016.
13. Smith DM, McLachlan KR, McCall WD Jr. A numerical model of temporomandibular joint loading. J Dent Res. 1986;65(8):1046-1051.
14. Hatcher DC, Faulkner MG, Hay A. Development of mechanical and mathematic models to study temporomandibular joint loading. J Prosthet Dent. 1986;55(1):377-384.
15. A technique for recording centric relation. Lucia VO. J Prosthet Dent. 1964;14:492-505.
16. Tarantola GJ, Becker IM, Gremillion H. The reproducibility of centric relation: a clinical approach. J Am Dent Assoc. 1997;128:1245-1251.
17. Barkley RF. Successful Preventive Dental Practices. Preventive Dental Press; Macomb, IL: 1972.
18. Pankey LD, Davis WJ. A Philosophy of the Practice of Dentistry. Medical College Ohio: 1985.
19. Lockhard MW. The Exceptional Dental Practice, Why Good Enough Isn’t Good Enough. Lockhard Publications: 2007.
About the Author
Edwin A. McDonald III, DDS
Private Practice
Plano, Texas